The human body speaks in whispers before it screams. Nowhere is this truer than in cardiovascular health, where inflammation serves as both protector and perpetrator. Long gone are the days when doctors viewed the cardiovascular system as mere plumbing; today’s research reveals an intricate biochemical dialogue where inflammation markers act as early warning signals. These molecular messengers tell stories of arterial stress, endothelial dysfunction, and brewing storms that could lead to heart attacks or strokes if left unchecked.
C-reactive protein (CRP) has emerged as the most studied inflammation marker in cardiology. Produced by the liver in response to interleukin-6, CRP levels rise when arteries develop atherosclerotic plaques. What makes CRP particularly valuable is its ability to predict cardiovascular events even in apparently healthy individuals. Studies show that people with high-sensitivity CRP (hs-CRP) levels in the upper third have twice the risk of coronary events compared to those in the lower third. This holds true regardless of cholesterol levels, suggesting inflammation operates on a parallel destructive pathway.
Beyond CRP, the cardiovascular system leaves other inflammatory breadcrumbs. Fibrinogen, a clotting factor that increases during inflammation, creates a dangerous double threat by both promoting blood clots and exacerbating arterial stiffness. Then there’s interleukin-6 (IL-6), the cytokine maestro that orchestrates multiple inflammatory responses. IL-6 doesn’t just stimulate CRP production—it directly damages endothelial cells, those delicate guardians lining every blood vessel. The endothelium’s struggle to maintain vascular homeostasis under IL-6 bombardment often manifests as elevated blood pressure and reduced nitric oxide availability.
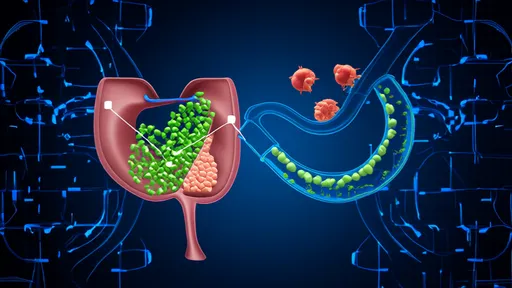
Modern medicine now recognizes that atherosclerosis isn’t merely cholesterol accumulation but an inflammatory process wearing the disguise of lipid storage. When LDL cholesterol particles oxidize within arterial walls, they trigger an immune response akin to fighting an infection. Macrophages rush to engulf these oxidized lipids, transforming into foam cells that form the fatty streaks of early atherosclerosis. This explains why statins, beyond lowering cholesterol, demonstrate anti-inflammatory effects that contribute significantly to their cardiovascular benefits.
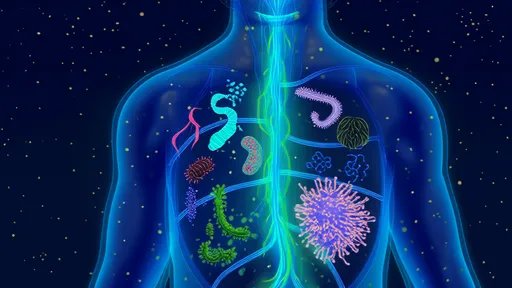
The gut-heart axis adds another layer to inflammation’s cardiovascular impact. Microbial imbalances in the intestine increase circulating lipopolysaccharides (LPS), endotoxins from gram-negative bacteria that provoke systemic inflammation. This microbial mischief manifests in elevated inflammation markers and appears particularly relevant in heart failure patients. Research reveals that heart failure progression correlates with intestinal permeability—the infamous "leaky gut"—allowing LPS to enter circulation and further strain an already struggling cardiovascular system.
Measuring these inflammation markers has transitioned from research labs to clinical practice, though not without controversy. While hs-CRP testing gained endorsement for intermediate-risk patients in cardiovascular guidelines, questions remain about whether lowering inflammation markers actually reduces risk or merely reflects it. The landmark CANTOS trial provided partial answers by showing that targeting IL-1β with canakinumab reduced cardiovascular events independent of lipid changes, offering proof that anti-inflammatory therapy could work—albeit with increased infection risk.
Lifestyle factors write their signatures across inflammation markers with remarkable consistency. The Mediterranean diet, rich in polyphenols from olive oil and flavonoids from berries, demonstrates measurable reductions in CRP and IL-6. Exercise, particularly aerobic activity, creates an anti-inflammatory environment through myokine release from working muscles. Even dental health plays a role—chronic periodontitis elevates systemic inflammation, explaining its association with coronary artery disease. These connections underscore that cardiovascular inflammation monitoring isn’t just about identifying risk but revealing opportunities for intervention.
Emerging technologies are pushing inflammation monitoring toward personalized thresholds. Machine learning algorithms now integrate multiple biomarkers with clinical data to predict individual inflammation trajectories. Wearable devices attempt to detect pro-inflammatory states through subtle changes in heart rate variability and skin temperature. Such innovations could transform inflammation from an abstract biomarker into a daily health metric as trackable as blood pressure.
The story of inflammation and cardiovascular health keeps unfolding with each research breakthrough. From the discovery of novel markers like galectin-3 in cardiac fibrosis to the recognition that resolving inflammation—not just suppressing it—may hold therapeutic promise, this field continues redefining how we protect hearts. What remains clear is that listening to inflammation’s whispers gives medicine its best chance to prevent cardiovascular disease from ever screaming.

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025

By /Jul 14, 2025
By /Jul 14, 2025

By /Jul 14, 2025